It's a scary-sounding diagnosis. But don't panic if you learn you have degenerative disc disease. In spite of its name, it's not actually a disease, and it doesn't inevitably worsen over time.
"The normal process by which discs change as we age is simply called 'degeneration.' So everyone experiences it to some degree during their lifetime," says Gregory Lopez, MD, an orthopedic spine surgeon at Rush.
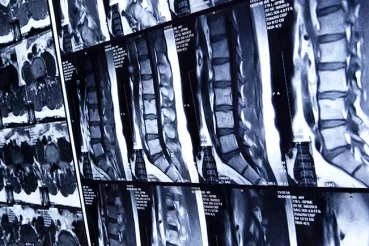
When discs deteriorate
As we age, our discs start to dry and shrink. In some cases, these changes lead to ruptured — or herniated — discs, instability in the spine, and/or narrowing of the spinal canal.
These issues may in turn cause symptoms, including neck pain or back pain, radiating pain, and weakness or numbness in the arms or legs.
The good news: Symptoms don't typically progress.
"A diagnosis in your 30s or 40s doesn't mean you'll be in a wheelchair by 70," says Matthew Colman, MD, an orthopedic spine surgeon at Rush. "In fact, with aging, the degenerative process sometimes burns out to a point where it causes less pain."
And taking steps to manage symptoms and keep your spine and back healthy can help you stay mobile and active throughout your life.
Prevention is the best medicine
A healthy lifestyle not only improves symptoms, it can actually slow the degenerative process. That's why Lopez and Colman recommend the following:
- Exercise. Make aerobic activities, core strengthening and stretching part of your routine, including working with a physical therapist if your doctor recommends it. Exercise can help you control your weight and keep your spine strong and healthy.
- Maintain a healthy weight. Being overweight puts more stress on your spine. It can also keep you from being physically active.
- Don't smoke. In addition to increasing your risk of heart disease, stroke, lung disease and cancer, smoking cigarettes can significantly affect disc health and speed the rate of degeneration.
- Drink more water, less alcohol. Hydration promotes healthy discs and a healthy body; excessive alcohol dehydrates. Heavy drinking can also lead to injury-causing falls or accidents. Stick to the recommended one alcoholic beverage daily for women, two per day for men. And take big sips of water between sips of alcohol to make your drink last longer and help prevent alcohol-related dehydration.
Managing the pain
Along with lifestyle changes and physical therapy, your doctor may prescribe medications to minimize painful flareups, including the following:
- Over-the-counter pain relievers (e.g., acetaminophen)
- Nonsteroidal anti-inflammatory drugs (e.g., ibuprofen) or cortisone injections
- Spinal injections (e.g., epidural steroid injections)
In addition to increasing your risk of heart disease, stroke, lung disease and cancer, smoking cigarettes can significantly affect disc health and speed the rate of degeneration.
When to have surgery
"Most people feel and function better once symptoms are treated by nonsurgical means and they have learned and committed to proper self-care," Lopez explains.
If your pain isn't improving or your symptoms are affecting your quality of life, however, your doctor may recommend surgery:
- Decompression – removal of a displaced disc or overgrown bone to free pinched nerves.
- Fusion – building a bone bridge to provide stability and prevent painful motion.
- Deformity correction to address abnormal curvatures.
- Placement of implants, such as spacers, artificial discs and nerve stimulators.
"There are many ways to address the symptoms resulting from disc degeneration," says Colman. "The key is to determine what's causing your symptoms and work with your spine specialist to find the right approach for you."