Autonomy has, as its basic components, personal accountability and shared power and influence. An autonomous nursing staff is feasible. It is professionally exciting. It cannot be done for nurses; it must be done by them.
— Luther Christman, PhD, RN, FAAN, first dean of the Rush University College of Nursing
Rush nurses never stop asking how things can be done better, transforming the way patients are cared for and improving the way Rush functions. Our strength is in shared governance and being empowered to transform how we deliver health care.
The shared governance model at Rush University Medical Center gives clinical nurses a voice in determining nursing practice, standards and quality of care.
This model, implemented in 1983, reflects the high professional stature of nurses at the hospital.
The advantages of shared governance are twofold:
- It empowers nurses to use their clinical knowledge and expertise to develop, direct and sustain our own professional practice.
- It allows nurses to network with colleagues and to collaborate among units and departments.
Professional Nursing Staff
At Rush University Medical Center, the Professional Nursing Staff (PNS) directs standards for nursing practice and care. PNS maintains standards, documentation and quality improvement, and helps create an environment that promotes the retention and recruitment of highly qualified professional staff.
The mission of PNS is as follows:
- To provide high-quality and cost-effective nursing care for patients
- To establish and monitor standards of clinical practice
- To promote excellence in professional performance among the nursing staff
- To facilitate the quality of professional life of its members
Within the shared governance model, PNS provides nurses a way to communicate concerns and work toward solutions that benefit everyone. At Rush University Medical Center, all nurses are members of PNS, and all nurses have a voice.
Professional Nursing Practice Model
Relationships and caring are the foundation of the Rush nursing practice model. Care is patient and family-centered and holistic in nature. The nurse-patient relationship is characterized by sensitivity, collaboration, intentional presence, communication and respect.
Our nurses bring knowledge, skills and abilities to their practice which are blended to meet the needs of the patient and family. The necessary skills include critical thinking, technical expertise and evidence-based practice.
Interwoven into each of these aspects is our focus on leadership, which is the core of the model. Leadership takes shape in each situation but differs in scope by nursing position. Rush nurses strive to continuously learn and grow in their nursing practice and to be accountable leaders in any clinical care team.
Mission, Vision and Strategic Plan
Rush’s mission is to provide the best health care for individuals and the diverse communities we serve through the integration of outstanding patient care, education, research and community partnerships.
The Rush nursing vision and strategic plan revolve around the following ideas:
The Best People
Our goal is to have a highly engaged nursing staff. To achieve this goal, we focus on the following:
- Succession planning
- Leadership development
- Collaboration with schools and universities
- Intentional hiring for Rush University Medical Center nursing behaviors
The Best Quality
To achieve this goal, we focus on the following:
- Top performance on all quality and safety measures
- Culture of safety
- Teacher-practitioner model
- Care delivery model
- Interprofessional education and practice, including simulation training
- Change management
- Innovation and performance improvement
- Research initiatives
Nationally Recognized Programs
To achieve this goal, we focus on the following:
- Increasing nurse certifications
- Achieving and maintaining accreditations and designations
Highest Value
To achieve this goal, we focus on the following:
- Resource management
- Supporting the value equation in the definition of nursing work
Join the Nursing Team at Rush
Visit our Careers section to learn how you can apply for a nursing position at Rush.
Collaborative Relationships
Rush Copley nurses work in an environment where they are empowered to help drive decisions for nursing practice and performance improvement. Nurses are a vital part of a health care team that strives for a common goal of care and healing for each patient.
Effective Team Communication
Rush Copley’s health care culture fosters respectful, effective communication throughout the organization. Nurses build strong, collaborative relationships with fellow nurses, interprofessional team members, physicians and other providers to work together to deliver extraordinary care that results in quality outcomes.
Physician engagement survey results place Rush Copley nurses in the top 25 percent of hospitals nationally for teamwork and physician respect for nurses' contributions to patient outcomes.
Shared Decision Making
The purpose of the Shared Decision-Making Model, referred to as “Partnership,” is to provide a structure for a professional work environment that reflects the desire to have the highest level of accountable patient care, and to increase the participation of nurses and patient care staff in decisions that affect their practice at Rush Copley Medical Center. Our partnership model empowers all members to have a voice in decision-making, thus encouraging diverse and creative input that will help advance and support the mission of Rush Copley.
Rush Copley Nursing Care Delivery Model
The Nursing Care Delivery Model represents the way patient care is delivered at Rush Copley Medical Center. The patient is featured at the center to emphasize the patient as our top priority and our focus on meeting individual patient needs and preferences. The interdependence of the key concepts are represented by the overlapping circles. The delivery model applies to all direct care nurses.
Rush Copley Nursing Professional Practice Model
The Nursing Professional Practice Model is intended to unify the Rush Copley nursing community and is for nurses in all areas and levels across the organization. Surrounding the nurse is a foundation of performance expectations. The outer circle represents the practice environment we work within to achieve organizational, clinical and professional excellence.
Partnership Participation
Nursing Executive Congress
The Nursing Executive Congress provides oversight for the shared decision-making structure to ensure engagement and sustainability of the model through evaluation and re-evaluation and communication of all activities and processes that affect the nursing community. The Nursing Executive Congress serves as a communication link between nursing, other disciplines and departments and ensures the Rush Copley mission, vision, and objectives are incorporated into the nursing mission, vision, and annual tactical plan. This partnership model demonstrates the structure of shared governance at Rush Copley.
Practice Congress
The Practice Congress provides oversight to nursing practice to ensure incorporation of evidence-based care into clinical practice. The congress facilitates coordination and communication of practice and workflow changes as well as interprofessional collaboration that drives the best patient outcomes. The members of this congress work in association with the Nursing Policy and Procedure Committee, which reviews, approves and revises policies and procedures where nursing care is delivered.
Leadership Congress
The Leadership Congress organizes and manages the resources of the nursing community. The Leadership Congress implements initiatives that promote quality patient care and support the Rush Copley strategic plan and budget through an aligned nursing strategic plan. It also monitors progress toward established goals and expected outcomes.
Research and Professional Development Congress
The Research and Professional Development Congress provides the framework to conduct nursing research and utilize evidence-based practice. The Research and Professional Development Congress will provide a forum to mentor others in the use of clinical research findings and evidence-based information/data, or to conduct research. The congress will establish a vision of identifying innovations to support the work environment, advance the profession and improve patient outcomes.
Patient Care Quality and Safety Congress
The Patient Care Quality and Safety Congress coordinates and oversees nursing and patient care performance improvement activities to support the Rush Copley mission, vision and strategic plan. The congress is responsible for monitoring of and compliance with nurse-sensitive quality indicators and regulatory requirements. The members collaborate with the Nursing Professional Practice Committee to ensure safe care and facilitate optimal patient outcomes.
Unit Partnership Congress
Our unit partnership provides a structure to communicate ideas and outcomes related to building and strengthening relationships of each hospital department where nursing is practiced. The Unit Partnership Congress’s goal is to improve quality and safety of the patient care experience and continually elevate the professional practice environment.
Nursing Professional Governance Organization (NPGO)
How is NPGO Organized?
The NPGO Standing Committees and NPGO Unit/Specialty Area Committees (UACs) are in communication and both report up to the NPGO Executive Committee and Nursing Administrative Committee, respectively. These committees report up to the NPGO President and Chief Nursing Officer, respectively. The NPGO President and Chief Nursing Officer report up to the Rush Oak Park Hospital Board of Directors and the ROPH CEO.
Every Nursing Practice Area is Represented
Executive Committee representatives
President, President Elect, 3Center, 6West, Ambulatory Clinics, APRNs, Cath Lab/IR, CNO, Employee Health, Endoscopy, ER, ICU, Nursing Education, Nursing Supervisors, OR, PACU, Quality, Rehab, Same-Day Surgery, Skilled Care Unit, Telemetry and Wound Care Clinic
NSGO standing committees
Peer Review Council, Evidence-Based Practice, Research and Education, Clinical Standards of Practice and Care, Staffing Nurse Advisory Board, Magnet Stars, Awards and Recognition, APRN Practice Council
NSGO unit/specialty area committees
3Center, 6West, Ambulatory Clinics, Cath Lab/IR, Endoscopy, ER, ICU, OR, PACU, Rehab, Same-Day Surgery, Skilled Care Unit, Telemetry, Wound Care Clinic
“As leaders, nurses must act as full partners in redesign efforts, be accountable for their own contributions to delivering high-quality care and work collaboratively with leaders from other health professions. Being a full partner involves taking responsibility for identifying problems and areas of system waste, devising and implementing improvement plans, tracking improvement over time and making necessary adjustments to realize established goals. In the health policy arena, nurses should lead decision making and be engaged in health care reform-related implementation efforts. Nurses also should serve actively on advisory boards on which policy decisions are made to advance health systems and improve patient care.”
Institute of Medicine, 2010
Officers
President: Alison Cersley
alison_m_cersley@rush.edu
Past President: Colleen Chierici
colleen_chierici@rush.edu
Treasurer: Beth Hale
elizabethmichele_hale@rush.edu
NPGO Documents and Resources
- NPGO Bylaws Document
- NPGO Code of Conduct
- NPGO Clinical Advancement Process
- Practice Evaluation and Professional Development
- Key articles (for full reference list, please see NSGO Manual for Evaluating Nursing Practice)
- Christman, L. (1976) The Autonomous Nursing Staff in the Hospital. Nursing Administration Quarterly. 1(1), 37-44.
- American Association of Critical Care Nurses. (2005) Standards for Establishing and Sustaining Healthy Work Environments.
- Institute of Medicine. (2010) Future of Nursing: Leading Change, Advancing Health Report.
- Clavelle, J., Weston, M., Porter O’Grady, T. and Verran, J. (2016) Evolution of Structural Empowerment: Moving from Shared to Professional Governance. JONA. Vol. 46: 6, pp. 308-312
NPGO Professional Practice Model and Care Delivery Model
How Our Identity Drives the Transformation of Practice and Care Delivery
We view these models as being two sides of the same coin: how we practice as nurses and how we deliver care within the team.
Rush Oak Park Hospital Professional Practice Model
The Professional Nursing Practice Model at Rush Oak Park Hospital is a picture of our practice identity. Relationships and caring encircle and support all that we do as ROPH nurses.
Technical expertise, evidence-based practice and critical thinking work in synergy, supported by the Professional Nursing Practice Model, to propel us as nurses toward leadership of the complex health care environment to meet the needs of our patients.
The Jean Watson Caring Care Delivery Model has been adopted at ROPH to assist our patients with gaining control and becoming more knowledgeable, thus promoting their health both within our walls and in their homes.
It is the theoretical foundation for our care delivery system which identifies how work is organized within the nursing team, how nurses are deployed and what each team member’s role is.
Supported by the constructs of the Jean Watson Care Delivery Model, nurses organize the activities of care around the needs and priorities of patients and their families.
Delivery and organization of care may differ between care settings; however, the components of carative factors, caring occasion, transpersonal caring relationship and patient- and family-centered care drive initiatives through all of the nursing and interprofessional teams. (Watson, 1979)
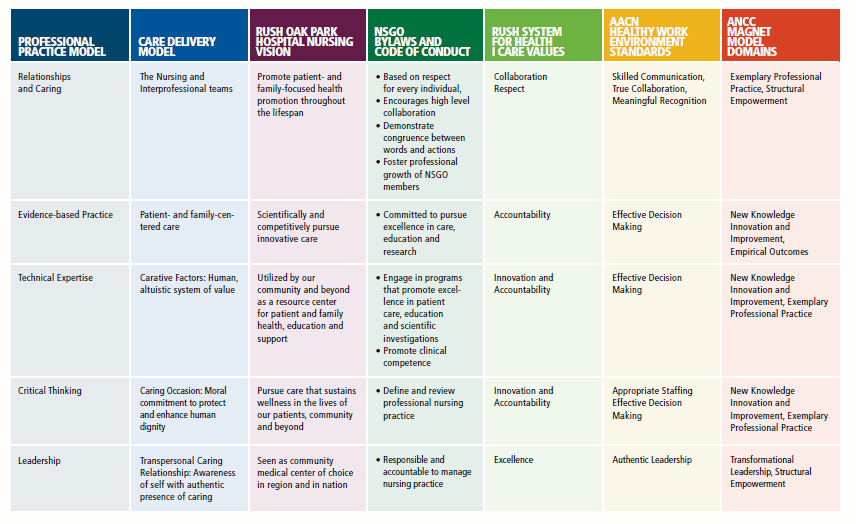
How Our Professional Practice Model Syncs With Other Important Structures: A Crosswalk
Nursing Professional Practice Model Evaluation Cycle
Wherever there is a nurse, the five domains of the practice models are driving description of practice, evaluation of practice and recognition of practice, as well as recruitment and retention of our practitioners.
All of these activities are done by and for nurses, with our discipline-specific standards, scope and body of knowledge. (click below image to enlarge)
Resources for Professional Development and Practice Evaluation
- Advanced Practice Registered Nurse Credentialing and Privileging Process
- Advanced Practice Registered Nurse Transition to Practice Manual
- NPGO Clinical Advancement Process
- New Nurse Orientation Pathway and Support Program
- Nursing Leadership Development Mentorship Program
- ROPH Performance Improvement Model and Evidence-Based Practice Guidelines
- ROPH Nursing Awards
- ROPH Nursing Resources: Publications, Websites, Literature, Certification, Professional Organizations, Colleges of Nursing Page 1 Page 2
- Illinois State Nurse Practice Act

