In July 2022, the RUSH University Medical Center Glycemic taskforce initiated significant changes to inpatient diabetes management to improve patient safety and reduce hypoglycemia. One notable change was to implement an insulin calculator that would determine the dose of insulin based on pre glucose levels and the percent consumed of the meal.
Insulin calculators as part of an electronic glucose management system show evidence of achieving safe glucose levels. The insulin calculator is a tool created in the electronic medical record (EMR) where clinical nurses input information regarding the percentage of the patient’s meal eaten, their current blood glucose level and the administration time. After entering the data, the calculator provides the dose of insulin to be administered by the clinical nurse.
The EMR build of the insulin calculator included all disciplines. It affected the inpatient flowsheets, and the insulin report was modified to include the calculator information. Testing of the calculator occurred and all disciplines including clinical nurses Emily Brey, Sarah Skeba and Karen Aicher, as well as members from the physician and pharmacy teams used the tool in the EMR playground to simulate workflows and evaluate the safety and accuracy of the tool.
Nurses from 9 Kellogg (medicine unit) provide valuable feedback to the team regarding how best to implement the insulin calculator to enhance workflow. The insulin dose calculator was completed in August 2022 and rolled out in October of that year.
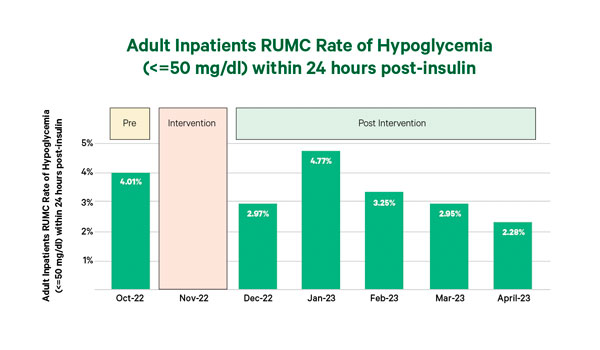
In October 2022, the rate of adult inpatients at the medical center who had a severe hypoglycemia event was 4.01%. The organization-wide change of adding the insulin calculator was a significant practice change. Since implementation, hypoglycemic events have decreased in patients that received insulin within the last 24 hours. The impact to patients is that it prevents extreme episodes of hypoglycemia and unstable blood sugar control.