History
A female patient in her 40s presented at an outside hospital as an urgent visit with metamorphopsias and blurry vision for one week. The patient was diagnosed with ovarian cancer two months prior to presentation and was currently receiving carboplatin and paclitaxel chemotherapy. She was responding well with significant reduction in CA125 levels, but started to develop visual symptoms one week after starting her first dose of chemotherapy. She was advised by her oncologist to get an eye exam.
Presentation and examination
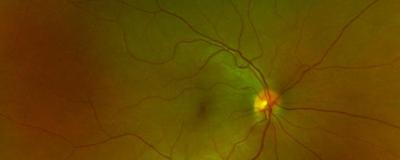
The patient’s ophthalmologic evaluation was remarkable with best-corrected visual acuities of 20/20 in the right eye and 20/40-1 in the left eye. The anterior segment exam was unremarkable, but the posterior fundus was significant for subretinal fluid in the macula in the left eye (Figure 1a) with corresponding areas of leopard patterned hypo-autofluorescence seen on autofluorescence photography (Figure 1b).
Figure 1
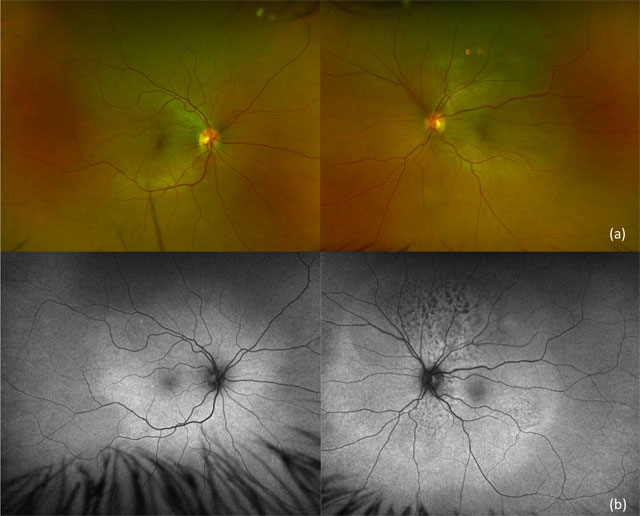
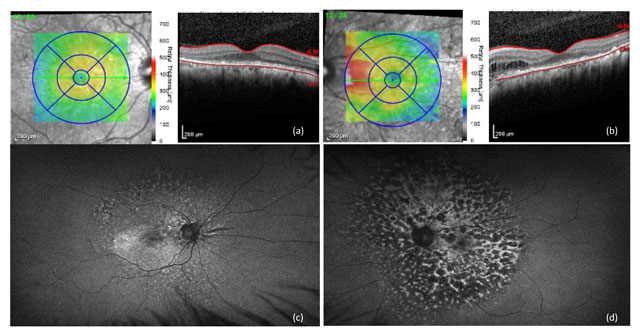
Optical coherence tomography (OCT) of the retina demonstrated a serous retinal detachment in the left eye (Figure 2a).
Figure 2
The infectious workup and MRI brain were unremarkable. High-dose oral steroids were started, but subretinal fluid continued to progress with binocular involvement (Figure 2b).
Best-corrected visual acuity deteriorated to 20/50+2 in the right eye and 20/150+1 in the left eye. At this time, there was concern for bilateral diffuse uveal melanocytic proliferation (BDUMP) given the patient’s history of ovarian cancer. The decision was made to admit the patient for plasmapheresis and for further oncology evaluation.
Treatment
The patient was started on an every-other-day course of plasmapheresis with significant improvement in visual acuity and a decrease in subretinal fluid (Figure 2c) after three rounds of treatment.
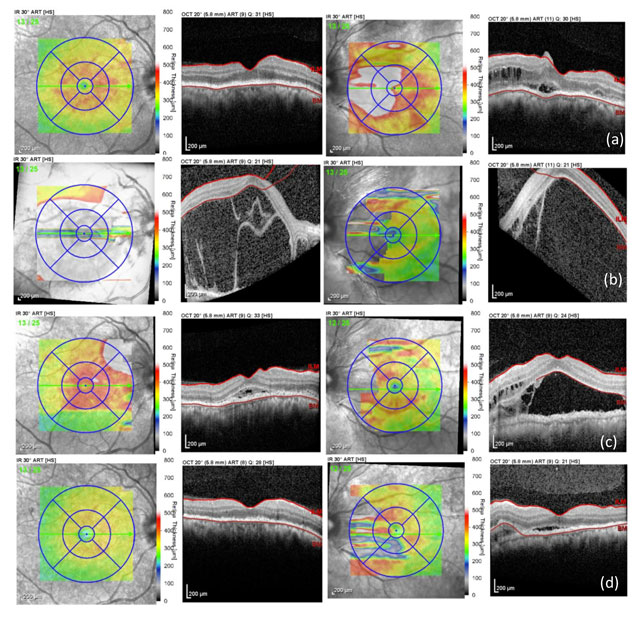
At this time, the patient started to develop nuclear sclerotic cataracts that were not present in the initial presentation. The patient continued to receive chemotherapy while admitted and was discharged with biweekly outpatient plasmapheresis. Her best corrected visual acuity was 20/30 in both eyes with minimal subretinal fluid on OCT (Figure 2d) on outpatient follow-up, but the leopard pattern lesions continued to persist on autofluorescence photography (Figure 3).
Figure 3
Outcome
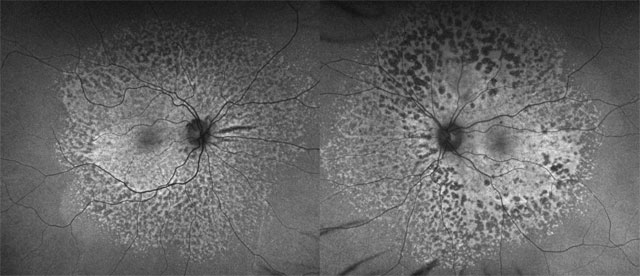
The patient subsequently underwent a successful total hysterectomy, salpingectomy, and oophorectomy. There was a decrease in frequency of plasmapheresis while the patient was recovering, and she developed worsening vision and recurrence of serous retinal detachment in the left eye. Once plasmapheresis was restarted three times per week, her vision improved, and the serous retinal detachment improved but at a slower rate than what was previously seen. Ultimately, the patient was slowly tapered off plasmapheresis over the course of several months and she continued to maintain her level of vision and continued resolution of her subretinal fluid (Figure 4).
Figure 4
Analysis
BDUMP is a rare paraneoplastic syndrome characterized by benign proliferation of choroidal melanocytes resulting in serous retinal detachments and severe vision loss. Unfortunately, it is also associated with high morbidity and mortality with survival rates ranging from eight to 24 months.[1] Given the rarity of this condition, there are no set treatment guidelines for the ocular manifestations of BDUMP.
The most successful treatment documented in the literature is plasmapheresis.[2] Plasmapheresis involves filtering the blood plasma with nonselective removal of proteins such as paraneoplastic antibodies. While there are no clinical trials demonstrating the efficacy of plasmapheresis in managing BDUMP, multiple case reports have demonstrated significant improvement in visual acuity and serous retinal detachments following this treatment.[2-8]
However, the interval, duration, and long-term efficacy of plasmapheresis for the management of BDUMP remains unknown. Our case demonstrated significant improvement in serous detachments following five rounds of plasmapheresis. Other documented cases required significantly more sessions to achieve clinical improvement.[3]
Interestingly, our patient experienced worsening vision and return of serous retinal detachment when plasmapheresis frequency was inadvertently decreased and improvement in both vision and serous retinal detachment when plasmapheresis was increased again to three times per week. This could suggest the need for plasmapheresis more frequently during times of stress. Therefore, plasmapheresis should be considered when treating patients with deteriorating visual acuity in the setting of BDUMP.
Oscar Chen, MD, MS, and Fred Crawford, MD, are resident ophthalmologists at Rush University Medical Center.
References
- O'Neal KD, Butnor KJ, Perkinson KR, Proia AD. Bilateral diffuse uveal melanocytic proliferation associated with pancreatic carcinoma: A case report and literature review of this paraneoplastic syndrome. Surv Ophthalmol. 2003;48(6):613-625. doi: 10.1016/j.survophthal.2003.08.005.
- Miles SL, Niles RM, Pittock S, et al. A factor found in the IgG fraction of serum of patients with paraneoplastic bilateral diffuse uveal melanocytic proliferation causes proliferation of cultured human melanocytes. Retina. 2012;32(9):1959-1966. doi: 10.1097/IAE.0b013e3182618bab.
- Mets RB, Golchet P, Adamus G, et al. Bilateral diffuse uveal melanocytic proliferation with a positive ophthalmoscopic and visual response to plasmapheresis. Arch Ophthalmol. 2011;129(9):1235-1238. doi: 10.1001/archophthalmol.2011.277.
- Jaben EA, Pulido JS, Pittock S, Markovic S, Winters JL. The potential role of plasma exchange as a treatment for bilateral diffuse uveal melanocytic proliferation: A report of two cases. J Clin Apher. 2011;26(6):356-361. doi: 10.1002/jca.20310.
- Navajas EV, Simpson ER, Krema H, et al. Cancer-associated nummular loss of RPE: Expanding the clinical spectrum of bilateral diffuse uveal melanocytic proliferation. Ophthalmic Surg Lasers Imaging. 2011;42:103. doi: 10.3928/15428877-20111020-02.
- Moreno TA, Patel SN. Comprehensive review of treatments for bilateral diffuse uveal melanocytic proliferation: A focus on plasmaphereis. Int Ophthalmol Clin. 2017;57(1):177-194. doi: 10.1097/IIO.0000000000000156.
- Jansen JCG, Van Calster J, Pulido JS, et al. Early diagnosis and successful treatment of paraneoplastic melanocytic proliferation. Br J Ophthalmol. 2015;99(7):943-948. doi: 10.1136/bjophthalmol-2014-305893.
- Schelvergem KV, Wirix M, Nijs I, Leys A. Bilateral diffuse uveal melanocytic proliferation with good clinical response to plasmapheresis and treatment of the primary tumor. Retin Cases Brief Rep. 2015;9(2):106-108. doi: 10.1097/ICB.0000000000000104.