Introduction
Muscle herniation involves muscle protrusion through an acquired or congenital fascial defect. Causes of acquired fascial defects are often from trauma (blunt or penetrating), strenuous exercise, or iatrogenic. This is more common in the lower extremity; upper extremity muscle herniation is rare, and as few as 30 cases have been reported in the modern literature (Roberts et al, Olch et al, Golshani et al, Khalid et al, Kozlow et al, Sanders et al, Hartmann et al, Tarrant et al, Lim et al, Schwartz-Fernandes et al, Ibrahim et al). The infrequency of this diagnosis may be related to absent or mild associated symptoms. Symptoms, if present, include soft tissue swelling, pain and cramping. Pain and size of the herniation may be provoked and increased by certain elbow, forearm or wrist motion as the muscle herniates through the defect during contraction. Rarely, herniation may irritate local traversing nerves, resulting in paresthesia or hypesthesia in the nerve’s anatomic distribution. The diagnosis can be made clinically with ultrasound or magnetic resonance imaging (MRI) (Kendi et al).
Treatment of muscular hernias includes reassurance, therapy, and, if severe or resistant to nonoperative treatment, surgery. Operative goals include primary repair of fascial defect or secondary reconstruction with autogenous flaps or allograft/synthetic material. Primary repair may not be possible in the setting of large defects or difficulty with mobilizing local fascia; therefore, reconstruction is a viable alternative option. Successful reconstruction with local or distant fascial flaps, mesh graft and acellular dermal matrices has been reported (Schwartz-Fernandes et al, Tarrant et al, Sanders et al, Kozlow et al). However, there is minimal literature on treatment of a symptomatic volar forearm muscle herniation with acellular dermal allograft in a pediatric patient. We report a case of median neurolysis and reconstruction of volar forearm fascial defect with acellular dermal allograft in a pediatric patient and review of the literature regarding this rare clinical scenario.
Case Report
History
A 10-year-old, right-hand dominant, healthy female sustained a closed right both bone forearm fracture in a gymnastics injury. She was closed, reduced and splinted in the emergency department on the day of injury, and was evaluated by a pediatric orthopedic surgeon one day later.
Displacement of the radius fracture was unacceptable at that time, and a recommendation was made for open reduction and internal fixation. The patient underwent successful open reduction and flexible intramedullary nailing of the radius three days following the injury. Of note, intraoperatively the interval between the flexor carpi radialis and brachioradialis was used to identify and reduce the radius fracture. She was treated in a cast for six weeks postoperatively, with uneventful and appropriate fracture healing. Removal of hardware occurred at eight months following primary surgery and injury, and the patient had full elbow, forearm and wrist range of motion at that time.
Presentation and examination
Two and half years following the initial surgery, the patient re-presented to the treating surgeon for a soft tissue mass in the volar aspect of the forearm, along the prior surgical incision site. The soft tissue mass was getting progressively larger over a span of months, with pain in the area, primarily with flexion and extension of the wrist during gymnastics. Workup of the mass was performed with magnetic resonance imaging and was unremarkable, with no identifiable muscle herniation.
The patient was referred to a fellowship-trained hand and upper extremity orthopedic surgeon for further evaluation and treatment. At the time of initial evaluation, a physical exam revealed a 2- to 3-centimeter volar soft tissue mass along the prior incision that increased in size with pronation and wrist flexion. Paresthesias were elicited with compression of the mass in the median nerve distribution.
Treatment options offered at that time included continuing nonoperative modalities; however, if median nerve symptoms progressed, neurolysis and fascial defect reconstruction would be the suggested operative procedure. The patient failed a seven-week trial of nonoperative treatment and elected to proceed with surgery approximately five years following initial treatment for the both bone forearm fracture.
Treatment
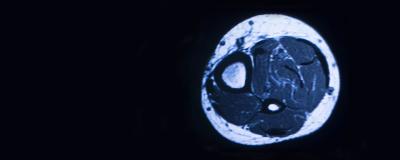
The prior incision along the volar aspect of the forearm was open, and median neurolysis was performed distally from the carpal tunnel proximal to the antecubital fossa. A 5-centimeter fascial defect was identified between the brachioradialis and the deep flexor muscles (Figure 1).
Figure 1

Intraoperative pronation demonstrated herniation through this fascial defect, that resolved in full supination (Figure 2, Video 1).
Figure 2

Provided the size of the defect and limited local donor tissue, an acellular dermal allograft was contoured and sutured with 2-0 braided, absorbable suture utilizing an inlay technique within the defect (Figure 3).
Figure 3

Following reconstruction, the muscular herniation with pronation resolved (Figure 4, Video 1).
Figure 4

The subcutaneous tissue and skin were closed with Monocryl in layers.
Outcome
Postoperatively, the patient had complete resolution of muscle herniation, pain and median nerve symptoms. At time of final follow-up six weeks postoperatively, all symptoms resolved with no recurrence of herniation and full return to gymnastics.
Discussion
Lower extremity muscle herniations are far more common than their upper extremity counterparts (Clinite et al, Huller et al, Harrington et al). This could be explained by higher intracompartmental pressures at baseline in the lower extremity with standing, walking and exercise compared to the upper extremity. Herniations frequently result from strenuous exercise, injury, congenital or iatrogenic.
The etiology of muscle herniation in this case is unclear, although it likely occurred at the time of surgical treatment for the initial fracture. Over time, as the patient grew, the defect likely increased, reaching a size threshold that allowed for forearm muscle herniation, especially as she increased muscular bulk participating in competitive gymnastics. Herniations are noticed but asymptomatic; however, symptoms may progress to pain and cramping during exercise as the muscle herniates along the fascial edge during contraction. Olch et al reported two requirements for symptoms to occur in forearm herniations, primarily based on location within the forearm. The fascial defect must be proximal enough to involve the muscle and not tendon, but distal enough for the proximal edge of the muscle to migrate against the fascial edge during contraction, which elicits inflammation and pain (Olch et al). Unique and infrequently reported symptoms include paresthesia and hypoesthesia of the traversing nerve in the region of the fascial defect. This finding was apparent in the case presented by Khalid et al, with a positive Tinel’s sign and alternated sensation in the median nerve distribution as a result of a flexor digitorum superficialis herniation. This finding was also present in our patient, specifically paresthesia of the median nerve distribution with compression of the herniation that resolved postoperatively.
Advanced imaging for muscle herniations includes ultrasound and MRI. Dynamic aspects of each of these modalities assists with identifying patients with vague or occult findings. The use of dynamic ultrasound is available and low cost, however, is user dependent. Kendi et al demonstrated dynamic MRI could also be utilized to determine size of muscle herniation and extend of the fascial defect. Interestingly, in this case, the MRI did not demonstrate a muscle herniation in our patient; however, it was apparent intraoperatively the herniation occurred in pronation and resolved in supination. This clinical scenario emphasizes the value a dynamic MRI contributes as it is not uncommon for these herniations to occur only with contraction of the affected muscle belly.
The majority of muscle herniations can be treated with rest, activity modification, compression wraps/sleeves and physical therapy modalities. Operative intervention is recommended in those that remain symptomatic and fail a trial of nonoperative treatment. Surgical options for herniations, regardless of location, include fasciotomy, direct closure, local and distant fascial flaps, or defect closure using grafts (Olch et al, Golshani et al,). The location and size of the defect will dictate the viability of the aforementioned options. Primary repair is simple and ideal for acute defects, however, Ibrahim et al reported success in a small series of patients presenting 4.6 years post-injury (Lim et al, Ibrahim et al). Although, direct closure of the fascial defect has been criticized by increasing risk for compartment syndrome (Olch et al, Miniaci and Rorabeck). An early series of patients demonstrated treatment with fasciotomy alone for forearm herniation resolved symptoms in less than half the included patients (n=3/7, 43%) (Olch et al). While fasciotomy is a reliable option for the lower extremity, outcomes are less predictable in the upper extremity and may be cosmetically unappealing.
Local fascial flaps can be harvested and mobilized for small defects in an area with appropriate and expendable donor tissue (Schwartz-Fernandes et al). More commonly, autogenous tissue is harvested from distant donor sites including from the fascia lata or palmaris longus tendon for defect closure (Roberts et al, Khalid et al). Different techniques have been described for use of fascia lata, including both inlay, onlay, and wraparound, with successful results in individual patients (Khalid et al). However, the pitfall to use autogenous tissue is donor site morbidity, especially in the pediatric patient population, as in our case.
Use of allograft or synthetic material has been successful in upper extremity herniations for a small number of cases including complete resolution of herniation and symptoms (Kozlow et al, Sanders et al, Hartmann et al, Tarrant et al). The safety profile of acellular dermal allograft has been established in humans, and its utilization continues to grow across many surgical subspecialties (Shorr et al, Rowe et al). They are widely available and can be utilized successfully for both large and small fascial defects while avoiding donor site morbidity (Kozlow et al). For these reasons we utilized acellular dermal allograft for the sizable defect in our pediatric patient, with successful resolution of the herniation immediately following defect closure.
Many novelties exist in this report. The majority of upper extremity muscle herniation occurs in adult men following strenuous activity or injuries. There are very few reports of pediatric upper extremity muscle herniations. To our knowledge, we present the first female, pediatric muscle herniation following a both bone forearm fracture and fixation. Furthermore, reconstruction was performed successfully with acellular dermal allograft, an infrequently reported allograft option thus far in the literature. We utilized acellular dermal allograft in this case provided its availability, size of defect, and avoidance of donor site harvesting. The patient achieved resolution of the herniation, pain and associated nerve symptoms with use of this technique, demonstrating it as a viable option for adults and pediatric patients with symptomatic, volar forearm muscle herniations.
References
- Roberts JO, Regan PJ, Dickinson JC, Bailey BN. Forearm muscle herniae and their treatment. J Hand Surg Br. 1989;14(3):319-321.
- Olch CL, Watson HK. Symptomatic forearm fascial hernia. J Hand Surg Am. 1996;21(4):693-695.
- Golshani SD, Lee C, Sydorak R. Symptomatic forearm muscle hernia: repair by autologous fascia lata inlay. Ann Plast Surg. 1999;43(2):204-206
- Khalid KA, Mah ET. Treatment of a symptomatic forearm muscle herniation with a wrap-around fascia lata graft. J Hand Microsurg. 2009;1(1):54-59.
- Kozlow JH, Beil RJ, Chung KC. Repair of symptomatic forearm hernias using acellular dermal matrix--two case reports. J Hand Surg Am. 2010;35(12):2053-2056.
- Sanders BS, Bruce J, Robertson J. Treatment of a symptomatic forearm muscle herniation with a mesh graft. Sports Health. 2011;3(2):179-181.
- Hartmann CE, Branford OA, Floyd D. Delayed repair in a case of forearm fascial muscle herniation using non-cross-linked acellular porcine dermal matrix. Tech Hand Up Extrem Surg. 2012;16(3):166-168.
- Tarrant SM, Hardy BM, Balogh ZJ. Repair of traumatic muscle herniation with acellular porcine collagen matrix. ANZ J Surg. 2014;84(6):464-467.
- Lim M-S, McInerney NM, Kelly EJ. Symptomatic non-traumatic muscle hernia in the dorsal forearm. JPRAS Open. 2015;3:26-28.
- Schwartz-Fernandes FA, Lew A, Gonzalez MD. Repair of Forearm Muscle Herniation Using Local Fascial Flap: A Case Report. Cureus. 2019;11(6):e4881.
- Abdel Hamid Ibrahim M, Ismail M, Taher Hassan Mohamed M. Muscle Hernias in the Upper Limb: Treatment and Literature Review. J Hand Surg Am. 2022;47(3):288.e281-288.e284.
- Kendi TK, Altinok D, Erdal HH, Kara S. Imaging in the diagnosis of symptomatic forearm muscle herniation. Skeletal Radiol. 2003;32(6):364-366.
- Clinite KL, Wyble A, Sugarman JL. Tibialis anterior muscle herniation in adolescents: A case series and review of the literature. Pediatr Dermatol. 2019;36(5):664-667.
- Hullur H, Salem Y, Al Khalifa J, Salem A. Tibialis anterior muscle hernia: rare but not uncommon. BMJ Case Rep. 2016;2016.
- Harrington AC, Mellette JR, Jr. Hernias of the anterior tibialis muscle: case report and review of the literature. J Am Acad Dermatol. 1990;22(1):123-124.
- Miniaci A, Rorabeck CH. Compartment syndrome as a complication of repair of a hernia of the tibialis anterior. A case report. J Bone Joint Surg Am. 1986;68(9):1444-1445.
- Shorr N, Perry JD, Goldberg RA, Hoenig J, Shorr J. The safety and applications of acellular human dermal allograft in ophthalmic plastic and reconstructive surgery: a preliminary report. Ophthalmic Plast Reconstr Surg. 2000;16(3):223-230.
- Rowe NM, Morris L, Delacure MD. Acellular dermal composite allografts for reconstruction of the radial forearm donor site. Ann Plast Surg. 2006;57(3):305-311.