History
A female patient in her 40s reported progressive dysphagia. She was diagnosed with esophageal adenoid cystic carcinoma at an outside hospital, where her medical team recommended an esophagectomy with laryngectomy for treatment. She came to RUSH for a second opinion.
Presentation and Examination
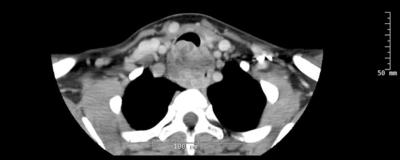
The patient had a large bulky tumor encasing the cervical esophagus, positive for low grade adenoid cystic cancer, which invaded the posterior tracheal wall over the length of 6 cm. The tumor was located 2 cm below the vocal cords and 3 cm above the carina.
We decided an esophagectomy with a gastric pull-up and an en bloc posterior tracheal wall resection with tracheoplasty would be the best course of treatment for this patient.

About adenoid cystic carcinoma
Adenoid cystic carcinoma (ACC) is a rare tumor of the head and neck. It most commonly occurs in the salivary glands and is rarely identified in the esophagus. ACC often has an insidious onset with vague symptoms and is characterized by perineural invasion and local recurrences. Approximately 200,000 people worldwide have this disease, 60% of whom are women. About 1,300 people are diagnosed with this type of cancer every year in the United States.
Treatment
The patient underwent a laparoscopic trans-hiatal esophagectomy, en bloc resection of the posterior tracheal wall with lymphadenectomy and a tracheoplasty. The trachea was transected below the first ring, and the posterior wall was resected along with the involved portion of the cervical esophagus down to the sixth ring. Given the location of the tumor, femoral veno-venous ECMO was used during the tracheal wall resection and reconstruction.
During the cervical dissection, we discovered that the tumor was involving both recurrent laryngeal nerves and thus were included in the en bloc resection. Once the specimen was removed, the left ansa hypoglossi was anastomosed to the remnant left recurrent laryngeal nerve. The remnant right recurrent laryngeal nerve was not amenable to anastomosis, so two branches of the right ansa hypoglossi were sutured to the posterior cricoid and thyroid arytenoid muscles.
The gastric conduit was anastomosed to the cervical esophagus using a single-layer, hand-sewn technique.
The final portion of the operation involved reconstructing the posterior tracheal wall. A Doppler was used to identify the supraclavicular artery along the right neck and deltoid. A supraclavicular pedicled fascial flap was then created, de-epithelialized, rotated 90 degrees and used to reconstruct the back wall of the trachea. The remaining anterior tracheal rings were advanced superiorly and sutured to the newly reconstructed posterior wall. A split-thickness skin graft was harvested to cover the supraclavicular defect.
A tracheostomy was then performed between the new 3rd and 4th tracheal rings. The patient did well postoperatively. She underwent bilateral vocal fold injection laryngoplasty. Her final pathology revealed a T4N0M0 adenoid cystic carcinoma with microscopically positive margins; she then completed adjuvant radiation therapy.


Outcome
The patient was recently seen and is doing well, with no evidence of recurrence two years after surgery. She was eventually decannulated after two subglottic dilations. She must pay a little closer attention to swallowing carefully but otherwise has normal function.
Analysis
Preserving the patient’s quality of life
To treat this patient’s tumor, an esophagectomy and laryngectomy was one option, but this would have left her without the ability to speak naturally and with a permanent stoma. The RUSH multidisciplinary team of cardiothoracic surgeons, ENT/head and neck surgeons, and medical and radiation oncologists worked together to allow her to keep her voice and swallow normally.
Three key factors enabled us to do this specialized reconstruction.
- The patient’s tumor was just low enough (2 cm) beneath her vocal cords to allow us to save her larynx and perform the posterior tracheal wall reconstruction.
- During the surgery, nerves to both of the patient’s vocal cords had to be cut. When that happens, patients are typically unable to breathe normally and become tracheostomy dependent. We were able to do bilateral nerve grafting from her ansa hypoglossi nerves, which maintained the paramedian position and muscle bulk of the vocal cords. Thus, we were able to preserve natural voice and eventually eliminate the stoma.
- The use of ECMO is uncommon during a procedure to reconstruct the posterior tracheal wall. Since we didn’t need to worry about operating around an endotracheal tube, we had enough time to rebuild her trachea.
- This patient’s overall excellent health allowed us to treat her in an aggressive and novel fashion. Patient selection is critical.